| Infections of the Nervous System IA Lecture Outline© Hanuš Rozsypal |
| Meningism | Lumbar puncture | CSF examination | Bacterial meningitis |
CLASSIFICATION OF NERVOUS SYSTEM INFECTIONS
- central nervous system
- meningitis
- encephalitis
- myelitis
- peripheral nervous system
- radiculitis
- neuritis
- combined involvement
- meningoencephalitis
- encephalomyelitis
- polyradiculoneuritis
- purulent
- aseptic
- specific
- acute
- subacute
- chronic
MENINGISM
- inflammation
- hemorrhage
- neoplasm
- increased intracranial pressure, high temperature etc.
- headache
- vomiting
- irritability, hyperesthesia, photophobia etc.
- meningeal signs
LUMBAR PUNCTURE
- To obtain CSF in a suspicion of meningitis
- Reduction of raised intracranial pressure
- Lumbar intrathecal instillation of drugs
- Mass lesion or very increased intracranial pressure (possible danger
of herniation - tentorial or cerebellar coning)
Some evidence for this circumstance are
- rapidly developing depression of consciosness (coma)
- focal neurologic signs
- convulsions
- papilledema.
- Significant coagulopathy (possible danger of bleeding)
- Infected lumbar area (possible danger of infection)
CSF EXAMINATION
- Cytology
- cell count
- Chemistry
- protein
- glucose
- chloride
- Microbiology:
- Gram´s staining
- latex agglutination
- bacterial cultures
- Serologic tests:
- Lyme disease serology
- Cytology:
- smear of the sediment
- immunocytology
- Chemistry:
- lactic acid
- colloidal gold curve
- oligoclonal bands
- immunoglobulins
- Microbiology:
- india ink
- fungal cultures
- mycobacterial studies
- electron microscopy (Borrelia burgdorferi)
- Virology:
- viral cultures
- PCR
- electron microscopy (JCV)
- Serologic tests:
- syphilis serology
CSF FINDINGS
|
Test
|
Item
|
Pattern | ||
| Normal | Purulent | Aseptic | ||
| Appearance |
|
pellucid | turbid | pellucid or haze |
| Cytology | Cell count (/3ml) | <10/3 | 1000-100000/3 | 10-1000/3 |
| Predominant cells | lymphocytes | polymorphonuclears | lymphocytes | |
| Chemistry | Protein | 0,1-0,4 g/l | 3-4 g/l and more | 0,4-1,0 g/l |
| Glucose | normal | low | normal | |
| Lactate | normal | high | normal | |
| Chloride | normal | normal | normal | |
| Microbiology | Gram stain | negative | positive (often) | negative |
| Latex agglutination | negative | positive (usually) | negative | |
| Bacterial culture | negative | positive (often) | negative | |
- Cell count: normal or low lymphocytar pleocytosis (<50/3ml)
- Protein: high (usually about 1g/l)
- Glucose: normal
- Chloride: normal
- Cell count: low mixed pleocytosis
- Protein: high
- Glucose: low
- Chloride: low
- Cell count: low mixed or polymorphonuclear pleocytosis
- Protein: high
- Glucose: normal
- Chloride: normal
Major causative organisms (90%)
- Streptococcus pneumoniae (pneumococcus)
- Neisseria meningitidis (meningococcus)
- Haemophilus influenzae
routes of infection
- hematogenous
- per continuitatem
- direct invasion (penetrating head trauma, meningomyelocele)
- Primary
- Secundary
- pneumonia (pneumococcus)
- head trauma - penetrating or closed (pneumococcus, staphylococcus, G- bacilli)
- chronic otitis media (pneumococcus)
- sinusitis (pneumococcus, Haemophilus)
- neurosurgery (G- bacilli, staphylococcus, anaerobes, Nocardia)
- CSF shunt (Staphylococcus epidermidis, S. aureus, G- bacilli, diphteroids)
- rapid onset
- fever
- headache
- vomiting
- confusion
- others: seizures, skin rash, myalgias
- fever
- meningismus
- skin rash (petechiae)
- other neurologic and related findings
- altered consciousness
- cranial nerve palsies
- signs of increased intracranial pressure (HR, BP, breathing, cranial nerves involvement)
- focal neurologic signs (hemiparesis, aphasia)
- other complaints
- herpes labialis
- signs of shock
- ESR: very high
- BC: leucocytosis
- CRP: very high
- CSF: polymorphonuclear pleocytosis, high protein level, hypoglycorrhachia
- cerebral abscess
- subdural and epidural empyema
- thrombophlebitis of venous sinus
- subdural effusion (hygroma subdurale)
- obstructive hydrocephalus
| Purulent Meningitis (Normal CT Scan) |
Cerebral Abscess * |
| Epidural Empyema * | Subdural Effusion ** |
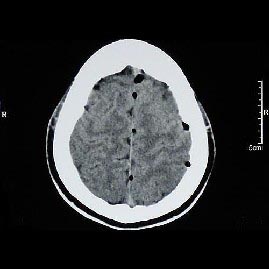 |
|
| Obstructive Hydrocephalus | Pneumocephalus |
- * Duniewicz M, Adam P, et al. Neuroinfekce. Maxdorf, Praha 1999, pp.309
- ** Táborská J, Koubová A, Valchová M. Hemofilové meningitidy u dětí do pěti let věku. Čes-slov Pediat 2002;57(3):91-100
- cranial nerve palsies
- motoric involvement (for example hemi- or quadruparesis, ataxia)
- myocarditis
- pericarditis
- metastatic or reactive arthritis
- disseminated intravascular coagulopathy (DIC)
- Watterhouse-Friderichsen´s syndrome
- pneumonia
- urinary tract infections (UTI)
- intravenous catheter-related bacteremia or sepsis
- fever (>4 days)
- behavioral disturbances, mental retardation
- visual problems
- hearing loss (deafness)
- motoric involvement (permanent paralysis)
- secundar epilepsy
- History: chronic otitis media and head trauma.
- Symptoms and signs: fever, headache, meningism and signs of cerebral dysfunction (declining level of consciousness).
- Laboratory data: CSF - pyogenic formula, ESR, BC, CRP - consistent with bacterial infection
- Additional examinations:
- Hemocoagulation
- Chemistry
- Blood cultures
- Fundoscopy (because excluding of papilledema)
- ENT exam
- X-ray (of chest, skull, mastoids, sinuses)
- CT scans, MRI, brain ultrasonography (in infancy)
- Audiogram
- Radioisotopic scanning
- Non-bacterial meningitis (aseptic, tuberculous, fungal)
- Brain abscess
- Intracranial or spinal epidural abscess/ empyema
- Subdural empyema
- Bacterial endocarditis with embolism
- Thrombophlebitis of venous sinus
- Ruptured dermoid cysts
- Brain tumors
Prognosis depends upon many factors, including the following:
- the causative microorganism
- the age of the patient
- the underlying diseases
- Antimicrobial agents:
| Age group | Common pathogens | Suggested regimens | Comments |
| Newborn | G- enteric bacilli, streptococci gr. B, D, Listeria monocytogenes | cefotaxime + ampicillin | |
| Infant 1-3 months | H. influenzae, S. pneumoniae, N. meningitidis, G- enteric bacilli, streptococci gr. B,D, L. monocytogenes | ceftriaxone/ cefotaxime + ampicillin | USA: + vancomycin *) |
| Infant 3 months to child to 7 years | H. influenzae, S. pneumoniae, N. meningitidis | ceftriaxone/ cefotaxime | USA: (+ vancomycin) |
| Ages 7-50 years | N. meningitidis, S. pneumoniae, L. monocytogenes | ceftriaxone/ cefotaxime or chloramphenicol | aqueous penicillin if dg. meningococcal meningitis is most-likely USA: (+ vancomycin) |
| Adult more than 50 years | S. pneumoniae, G- enteric bacilli, P. aeruginosa, L. monocytogenes | ceftriaxone/ cefotaxime (+ampicillin) | USA: (+ vancomycin) |
| Predisposing factor | Common pathogens | Suggested regimens | Comments |
| Alcoholism or other debilitating disease | S. pneumoniae, G- enteric bacilli, P. aeruginosa, L. monocytogenes | ceftriaxone/ cefotaxime (+ ampicillin) | USA: (+ vancomycin) |
| Head trauma, post-neurosurgery | S. pneumoniae, S. aureus, G- enteric bacilli, P. aeruginosa | chloramphenicol | USA: vancomycin + ceftazidim |
| Ventriculo-peritoneal or ventriculo-atrial shunt | S. epidermidis, S. aureus, G- enteric bacilli, Propionibacterium acnes | vancomycin + rifampicin or 3rd-gen. cephalosporin | |
| Chronic meningitis | M. tuberculosis, C. neoformans, neoplasm | No urgent empiric therapy | |
| HIV positive | C. neoformans, M. tuberculosis, T. pallidum, L. monocytogenes, S. pneumoniae, H. influenzae | ceftriaxone/ cefotaxime + ampicillin (+amphotericin B) |
- Reduction of intracranial pressure:
- Mannitol 20% (0.25g/kg q4-6h IV = 1.0-1.5ml/kg q4-6h IV)
- Dexamethasone (0.15mg/kg q4-6h IV)
- (Hyperventilation)
- Other supportive care and symptom-based therapy
- Infusions
- Antipyretics
- Anticonvulsants
- Mechanical ventilation
- Treatment of complications
- H. influenzae: H. influenzae type b (Hib) conjugate vaccine
- N. meningitidis: quadrivalent meningococcal vaccine (active against serogroups A, C, Y, and W135)
- S. pneumoniae: 23-valent pneumococcal vaccine
- S. agalactiae: not possible
- Basilar skull fracture: 23-valent pneumococcal vaccine (?)
- H. influenzae: (rifampicin)
- N. meningitidis: penicillin, co-trimoxazole, macrolids, rifampicin, ceftriaxone, ciprofloxacin
- S. pneumoniae: (penicillin, rifampicin)
- S. agalactiae: (ampicillin or penicillin intra partum)
- Basilar skull fracture: not recommended (?)
The page was last updated 20-April-2004